The Four Pillars of Safe Breastmilk Sharing
Introduction
Since 1991, fostering milksharing between families within her community was a normal occurence for Shell Walker Luttrell, retired LM, CPM in Arizona. It was not uncommon for people to call on her if their baby had a need for donor milk and as an organic response to this interesting calling, Shell established Eats on Feets on Facebook in July of 2010.
In October of 2010, Eats on Feets rapidly grew beyond Shell's personal community and became the first worldwide network of its kind using a social media platform. Shell and Maria, founders of the network, were filled with endless questions: Is milksharing really safe? Do families have access to the information that they need? Are babies being well served?
Together they delved into the research on human milk, pathogens, handling guidelines, milk bank policies and regulations, pasteurization, and much more. They logged over two thousand hours of research, communication with scientific authors, and consultations with experts, and gathered and organized the information that families and professionals need to safely share, or support the sharing, of breastmilk.
The result of their extensive research is gathered on the website Resource for the Informed Sharing of Human Milk. This Resource is a searchable database that offers families and professionals in-depth information on safe milksharing.
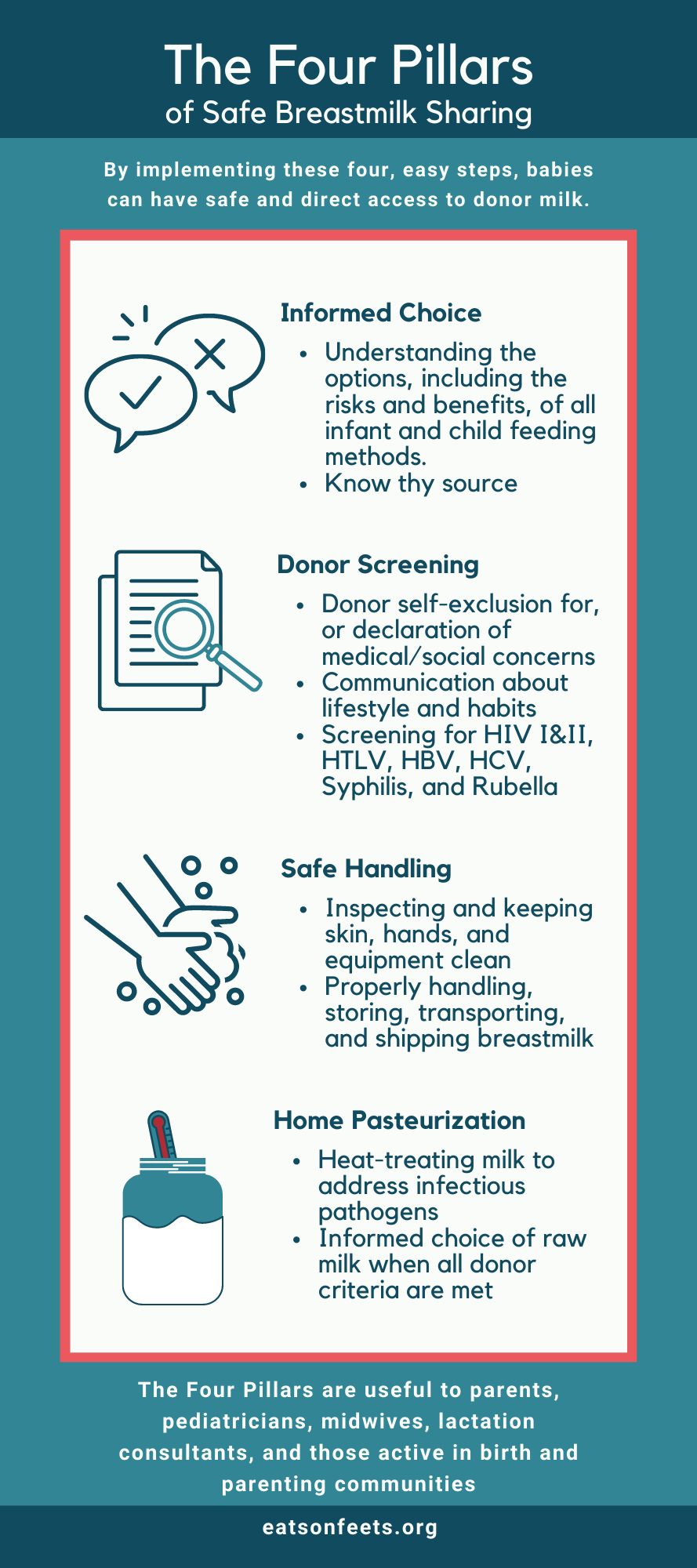
As a result of their work, the Four Pillars of Safe Breastmilk Sharing emerged: Simple to implement steps that form the foundation of safe community-based milksharing.
What are the 4 Pillars?
- 1. Informed Choice
- • Understanding risks and benefits, of all infant and child feeding methods
- • Know thy source
- 2. Donor Screening
- • Donor self-exclusion for, or declaration of, medical and social concerns
- • Communication about lifestyle and habits
- • Screening for HIV I and II, HTLV I and II, HBV, HCV, Syphilis, and Rubella
- 3. Safe Handling
- • Inspecting and keeping skin, hands, and equipment clean
- • Properly handling, storing, transporting, and shipping breastmilk
- 4. Home Pasteurization
- • Heat treating milk to address infectious pathogens
- • Informed choice of raw milk when all donor criteria are met
© eats on feets
1. Informed Choice

An informed choice is made by examining all credible, verifiable, and relevant information available and using it to carefully and objectively weigh options as well as potential consequences. When parents or professionals look for information in order to safely share breastmilk or support breastmilk sharing, it is important that ALL of the information is taken into consideration (not just those which supports personal dogma in regards to breastfeeding), in order to make truly informed choices.
To date, milk banks have set the standard for milksharing. Unfortunately, these standards are based on blood bank safety protocols, as breastmilk is considered a potentially infectious bodily fluid. Also, in certain situations or "non-normal" circumstances (such as cultural or religious need for donors to be identified, or for special dietary considerations), informed parents may choose to deviate from the milk bank standards in order to provide breastmilk in such a way that will allow them to maintain their beliefs or to suit their unique circumstances.
Informed health care providers should support and respect the individual rights of parents to make their own decisions about milksharing. Deviation from the standard is and should be a matter of personal and informed choice.
2. Donor Screening
Donor screening is based on three elements: donor self-exclusion, health and lifestyle communication, and blood testing. Proper donor screening reduces exposure to potential disease- and non-disease causing contaminants in breastmilk.
Donor Self-Exclusion Criteria
Health
- • Poor general health
- • Suffering from severe psychiatric disorder(s)
- • Confirmed positive for HIV I, HIV II, HTLV I or HTLV II
- • At risk for HIV (incl. sexual partner)
- • Current outbreak of herpes or syphilis lesion
- • Current open sores, blisters, and/or bleeding cracks on the skin
- • Undergoing chemotherapy or radiation treatment
- • On medication contraindicated for breastfeeding
Lifestyle
- • Currently abusing drugs, alcohol or OTC
- • When donating to a premature or critically ill baby:
- - Drinking, smoking, using certain herbal supplements or taking megavitamins
Social
- • Feeling coerced
- • At risk due to religious/social conventions
- • Undue stress on themselves or their family
Other
- • Having difficulty meeting needs of their own baby
- • Not meeting recipient criteria/request
3. Safe Handling

While some viral diseases, like Hepatitis B (HBC) and Hepatitis C (HCV), are not passed via breastmilk, contamination can occur when there are lesions and open sores anywhere on the skin. Breasts and body should be inspected for lesions, infectious blisters and bleeding nipples before expressing milk, and hands should be diligently washed before expressing milk and handling milk, milk collection equipment and supplies. Bacterial contamination of breastmilk can occur due to improper handling of pumping and storing supplies and of breastmilk. Parents can educate themselves about proper handling techniques and follow generally accepted guidelines for storage, transport and shipping of expressed milk.
4. Home Pasteurization
There are two methods of pasteurization that are safely and easily done at home: Low Temperature Long Time (LTLT) like the Holder method and Pretoria Heating, and High Temperature Short Time (HTST) like flash heating.
Holder pasteurization is the method used by most US milk banks. It can be performed in the home using a marketed single bottle pasteurizer. Pretoria Heating is done on the stove top, and is used in resource-poor areas for HIV positive lactating parents. These methods have been demonstrated to kill a wide variety of viruses and bacteria. However, they also have been shown to denature the milk of much of its nutritive properties, many of which may be especially beneficial for premature infants.
Flash heating, not to be confused with commercial flash pasteurization, was also developed for use in resource-poor areas for HIV-positive lactating parents. Flash heating can be accomplished on the stovetop or other direct heat source. Flash heating has been demonstrated to kill HIV, but its effect on other viruses is theoretical. Due to its relatively lower exposure time, this method has been demonstrated to preserve more of the milk's nutritive qualities than the LTLT methods.
Spore Forming Bacteria
It is important to note is that any pasteurizing of breastmilk raises the risk of spore release from spore-forming bacteria, like Bacillus cereus (B. cereus). While B. cereus is less of a concern for healthy-term babies, it can pose a significant risk to premature babies or those with gastrointestinal issues. This makes a good case for using raw milk from a thoroughly screened donor, and raw milk should also be taken into consideration for feeding premature or sick infants.
Raw Milk
Many families will prefer to use raw, unpasteurized milk so that their babies receive milk with greatest nutritional value. In the case of using raw donor milk, it is imperative for the recipient-donor relationship to be well established and/or for the donor to be thoroughly and recently screened. If this is not the case, the recipient may choose to pasteurize the milk.
Overview of both pasteurization techniques compared to raw milk
← Scroll to see full table →
| Temperature | Time | Efficacy | Results | Spore-formation | |
|---|---|---|---|---|---|
| Holder Pasteurization | 62.5°C (144.5°F) | Temp. is held for 30 minutes | Virtually eliminates the threat of viral and bacterial contaminants | - Some decrease in bacteriostatic properties - Lipase destroyed - IgA reduced by 70% - Lactoferrin reduced by 40% - Post heat treatment increase in thiamin, riboflavin, vitamin B6, folate, and vitamin B12* | Potentially |
| Pretoria-heating | 62.5°C (144.5°F) | Temp. is held for 20-30 minutes | - Virtually eliminates HIV but less effective than Flash-heating - Less inhibition of E.coli and S. aureus than Flash-heating - Other pathogens not directly addressed | - Some decrease in bacteriostatic properties assumed - Reduced but biological activity of lactoferrin not impaired - Post heat treatment increase in thiamin, riboflavin, vitamin B6, folate, and vitamin B12* | Potentially |
| Flash-heating | 72°C (161.5°F) | – Milk is exposed to this heat for a few seconds - Whole process takes +/-5minutes | - Virtually eliminates HIV, E. coli and S. aureus - Other pathogens not directly addressed | - Some decrease in bacteriostatic properties - Lipase significantly reduced assumed - IgA mostly intact - Reduced but biological activity of lactoferrin not impaired - Post heat treatment increase in thiamin, riboflavin, vitamin B6, folate, and vitamin B12* | Potentially |
| Raw (fridge) | 4°C (39°F) | - Milk may contain pathogens if from unscreened donor - CMV gone in 7 days when refrigerated | - No decrease in bacteriostatic activity - Lipase activity breaks down milk fats - Anti-infective properties intact | None | |
| Raw (frozen) | -15°C (5°F) | - Milk may contain pathogens if from unscreened donor - CMV virtually gone in 3 days when frozen | - Bacteriostatic properties 66% by 3 months - Lipase breaks down milk fats - Anti-infective properties intact | None |
© eats on feets
*We have not found any research to indicate that this is a positive result.
Safe Community Breastmilk Sharing
Safe and conscientious milksharing does not stop at medical screening, proper handling and pasteurization. Donors are often invested in the milksharing relationship on a more intimate level. Pumping or expressing milk is time consuming and donors who dedicate themselves to freely give their milk are nothing short of miracles to their recipients.

A parent-to-parent milksharing network can also be vital for a fast mobilization of aid in emergencies. Identifying key decision makers who influence infant and young child feeding practices at household, community and local health facility levels is crucial information when determining the priorities of action and response in emergencies.
Supporting safe community breastmilk sharing has far reaching benefits, and through milksharing, we can all contribute to infant, family, community, and ultimately, global health.
Please see the Eats on Feets Resource for Informed Breastmilk Sharing for in depth safety information.
Please feel free to share the PDF version of the above, the Midwifery Today article, and any of our shareable safety images in your community to help spread the word about safe community-based milksharing!
